Home » DeMystifying COVID Mortality: The Weight of Evidence
DeMystifying COVID Mortality: The Weight of Evidence
There are many potential explanations. Colleagues and I at the True Health Initiative have assembled a quite vast, global data set spanning biomarker, demographic, economic, social, and policy variations along with variations in COVID outcomes. The rather arduous work of making sense of it is under way.
In his thoughtful, initial exploration of the topic, Mr. Leonhardt considered a range of potential explanations, including some that are clearly correct, such as global variations in age distribution. We have known from the very earliest days of the pandemic that SARS-CoV-2 preys preferentially on the elderly, and the countries suffering the lowest casualty counts tend to be considerably younger, on average, than those bearing the brunt of loss.
Still, Mr. Leonhardt’s initial ruminations on the mystery of COVID mortality overlooked the one I have railed, repeatedly, resides in our cultural blind spot: the pandemic of obesity and chronic disease that was here all along.
Obesity has long been identified as a major risk factor for adverse COVID outcomes, a matter Mr. Leonhardt takes up in his return to the “mystery” topic today. In his comments, he cites the work of my colleague, Mary Adams, who has been contributing to our understanding of the links between our prior “pandemics” and this one right along– and gaining some attention from the New York Times into the bargain.
In her latest effort, Mary examined a global data set to reveal a strong association between obesity and the toll of COVID in countries with both high, average, per capita income, and high rates of obesity; but lack of association in countries with low income and low obesity prevalence.
So, is obesity causally implicated or not? I believe it is, and will explain why momentarily. But first, let’s give doubt its due.
In affluent countries like the U.S., obesity is worst among those socially and economically disadvantaged- so some, or theoretically even all, of the ill effects of obesity on COVID outcomes might be due to the company obesity generally keeps. Obesity and bad COVID outcomes might be “correlation without causation,” if something else associated with both- lack of access to good medical care, for instance- is the actual causal agent. Such agents in epidemiology are known as “confounders.”
In relatively indigent countries, perhaps obesity signifies lower risk for individuals- because the individuals vulnerable to obesity tend to have social and economic advantages relative to the population at large. Here, obesity might correlate with better access to good medical care, less crowding, and so on.
The case for such doubt is relatively weak, however. A contribution of obesity to COVID risk is a recurrent theme in research on the topic, and thus- epidemiologically consistent. The CDC just reported a clear dose-response relationship between BMI and COVID risk, a finding supportive of causal influence. There are, as well, clearly plausible pathways for the putative effects.
The mechanisms of an obesity influence on COVID severity are likely both metabolic (e.g., inflammation, impaired immune responses, compromised vascular health, endocrine imbalance, etc.) and mechanical (i.e., severe obesity compresses the thorax, reduces respiratory tidal volume, makes repositioning difficult). When I volunteered on the front lines in NYC during the surge, I saw that latter effect very clearly; there was an immediate benefit in oxygenation with repositioning, and with severe obesity, it was very hard- for patient and staff alike- to achieve that on an emergency department gurney.
Where obesity is scarce, it is not correlated with COVID outcomes- but that does not mean it is not influencing outcomes in individuals. An ecological analysis looks at the level of “A” and the level of “B” in the same population, but cannot say whether they are occurring in the same people. Obesity may contribute little to the population toll of COVID where obesity is relatively rare, yet still contribute quite a lot to the risk of those rare individuals affected.
There has long been reference to a particular “obesity paradox” that has largely been debunked – the notion that obesity at times confers a health advantage. Other things being equal, it does not.
But there is another, global, obesity paradox that has much clearer validity: obesity tracks with the opportunities of affluence in relatively indigent populations, but tracks with the burdens of indigence in affluent societies.
There is an epidemiologic reckoning with COVID19 still to come, a careful analysis of vast assemblies of data that will take time. As noted, colleagues and I will make our own, modest contributions to that worldwide effort.
Here in the United States, obesity is most severe where social, economic, and environmental disadvantages (not relative lack of will-power or personal responsibility!) make it so. Unbundling the specific contributions of these various factors to COVID risks and losses is nuanced and subject to on-going effort. When that effort is done, I predict with confidence that the charges against obesity will persist.
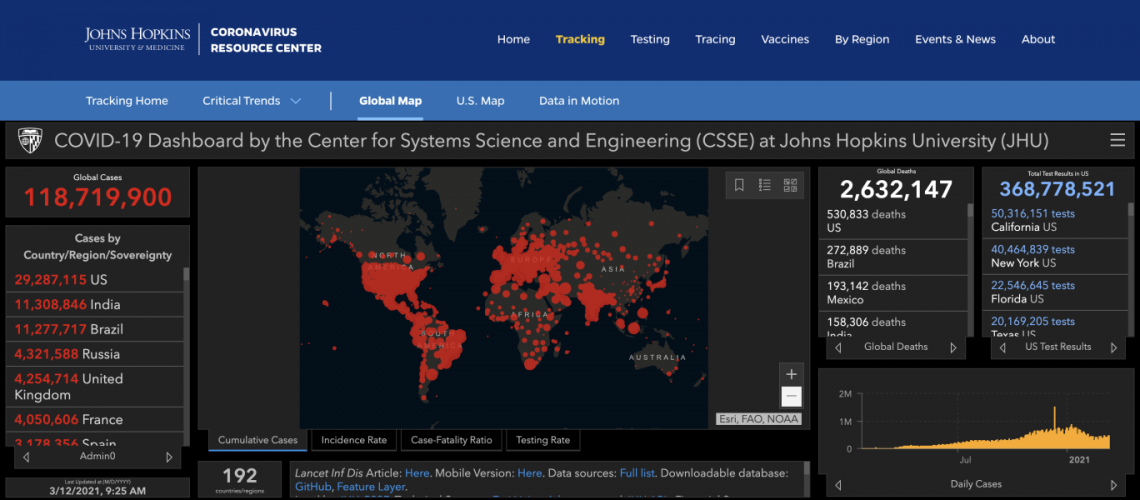
The weight of evidence is already more than ample to indict, if not convict, the prior pandemics of chronic, cardiometabolic disease and obesity as accomplices to the grim assaults of COVID19. Moreover, in the United States, where the over 500,000 losses to COVID we have suffered rightly garner collective, reverential sorrow – these antecedent pandemics claim more losses to premature death among us every year. Poor diet quality alone, a parameter over which we exercise total control- causes 500,000 or more premature American deaths annually. Yet these “prior pandemics”- which killed hundreds of thousands of us yearly on their own, then aided and abetted SARS-CoV-2 in killing hundreds of thousands more of us over the past year – garner no respect, no collective mourning, and arguably, little notice at all. They have been consigned to the background noise of epidemiology. We don’t hear them. We don’t see them.
Why? Perhaps, in part, because these are generally slow-motion perils that elude the fast-action potentials of the human fight or flight response. Perhaps, in part, because familiarity breeds contempt, even for the causes of mass casualties. Or, most disturbingly, perhaps because the propagation of obesity and chronic disease is very good business in America; costly for the many, but highly lucrative for the few. Perhaps the massive marketing might of those relative few has effectively whispered us into the trance that consigns this carnage to the acceptable background noise of modern epidemiology, allows the perpetrators of so much perennial loss to hide in plain sight.
Let that, too, figure in the reckoning due COVID19. In response to our grave losses, I sound the preventionist’s lament: we should not direct all of our resources to the consequences while neglecting the causes.
We have long done exactly that. We have long had the knowledge required to prevent fully 80% or more of the chronic disease burden that takes life from our years, the premature deaths that take years from our lives. Yet we have not translated that knowledge into the power of routine action. Quite the opposite- we have looked on complacently as these crises have worsened over time. COVID has appended the acute case for chronic health, yet health promotion and the amelioration of cardiometabolic liabilities have had no place to date in the national dialogue or principal policy responses.
If we are to wrestle with a “mystery,” it is not why our losses to COVID have been so high; that hides in plain sight. The mystery is our tolerance for the causes of such losses, this year, year in and year out, in deference to an usurious status quo. The mystery is our complacent neglect of the power to act based on knowledge long at our disposal.
The mystery, quite simply, is not want of explanation; it is want of outrage.
-fin
This article was first published on LinkedIn.
Dr. David L. Katz is a board-certified specialist in Preventive Medicine/Public Health
Click here to access the one-page summary of #TotalHarmMinimization
Click here to access the total harm minimization resource library
Click here to access a library of Dr. Katz’ “reality check” videos on the pandemic